|
Housingclick to view |

|
Health Careclick to view |

|
Child Care and Educationclick to view |

|
Technologyclick to view |

|
Foodclick to view |

|
Taxesclick to view |

|
Transportationclick to view |
||
Introduction
Poor health can be both a consequence and a cause of financial instability. ALICE and poverty-level families are more likely to become ill because their basic needs for health insurance coverage and regular, quality preventative care are not being met. They also have more difficulty recovering from illnesses both physically and financially. One illness or emergency can force a family into poverty.1
Even for people trying to make healthy decisions, health behaviors (like tobacco use, diet, and exercise) only account for about 30 percent of health outcomes.2 Other factors include access to care; economic factors like employment and income; and environmental factors like housing, air/water quality, and community safety.3
Issues in any of these areas can lead to chronic stress (often called “toxic stress”), which can impede a person’s ability to perform well in school, at work, and in daily life. This is especially true for young children: Adverse childhood experiences (ACEs) are known risk factors for poor health outcomes including depression, risky behaviors, and suicide, and are associated with lower life satisfaction.4
Cost is the major reason families do not have health insurance, and low-income people and people of color are at the highest risk of being uninsured.5 The Affordable Care Act (ACA) has made health insurance more accessible and affordable for millions of people: With the ACA’s expansion of Medicaid coverage, the national uninsured rate fell from 17 percent in 2013 to 10 percent in 2016. However, these gains reversed in 2017, when premium- and out-of-pocket costs increased, and the law to eliminate the health insurance mandate was passed. That year, the number of uninsured people increased by nearly 700,000, including 276,000 children.6
Uninsured adults are four times as likely as those with coverage to delay or forgo care, often waiting to seek treatment until an illness is advanced or pain is unbearable. Because half of all uninsured people have no usual source of care, many go to the emergency room for help because they have no other affordable, accessible options.7
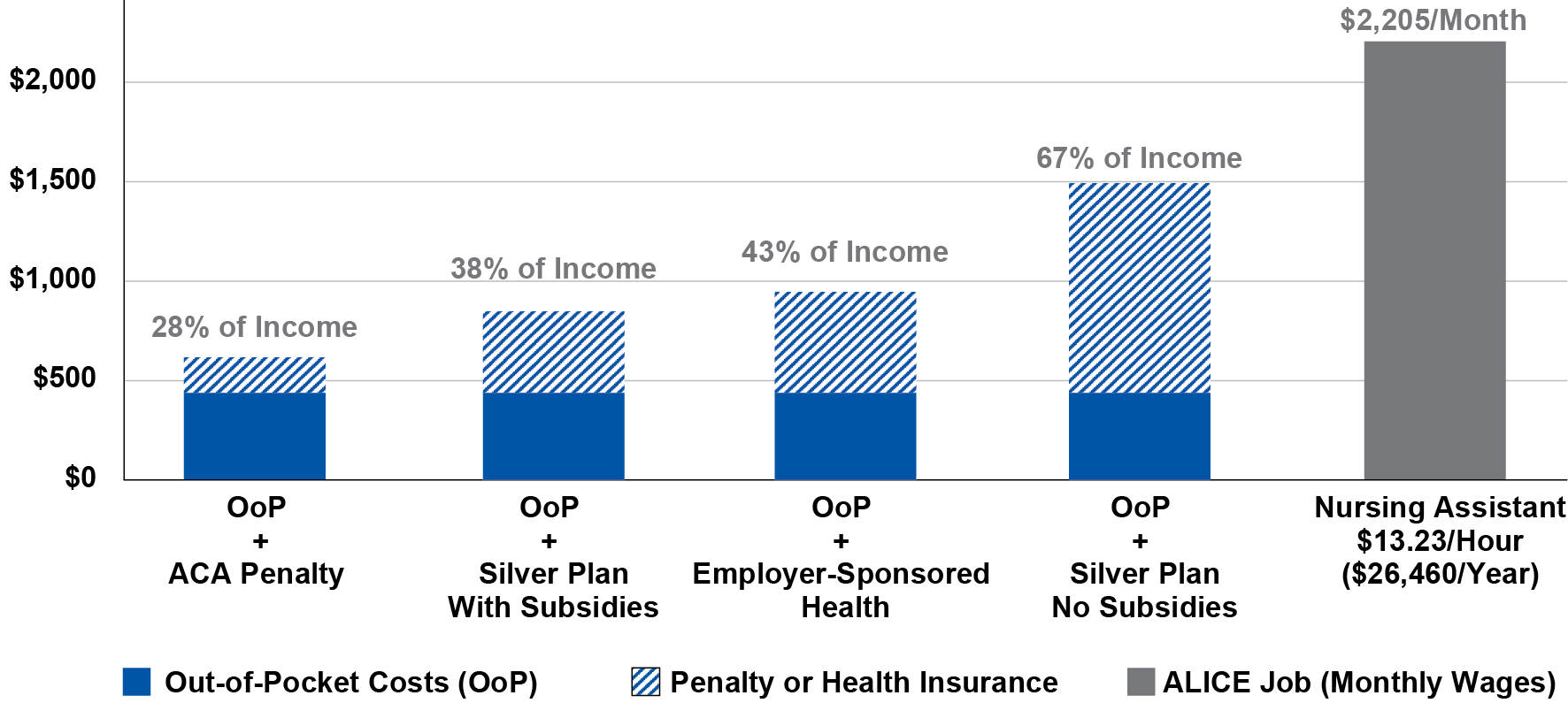
The gap between how much ALICE families need for health care and what they can afford to spend can be seen in the figure below, which compares four different monthly health care budgets for a family of four to the monthly salary of a full-time employee working as a nursing assistant. In 2017, more than 1.4 million ALICE workers across the U.S. had health care support jobs and earned an average hourly wage of $13.23, or $26,460 annually (if full time, year-round).
Out-of-pocket costs are represented by the dark portion of each bar. The health care budget includes the nominal out-of-pocket health care spending on insurance, medical services, prescription drugs, and medical supplies using the average annual health expenditure reported in the Consumer Expenditure Survey (CES).
Monthly Health Care Costs and Percent of an ALICE Income, U.S., 2017
Sources: Bureau of Labor Statistics. (2017). Occupational employment statistics: OES data. U.S. Department of Labor; Bureau of Labor Statistics. (2018, September). Consumer expenditure survey (CES): Table 3443. Consumer units of four people by income before taxes: Average annual expenditures and characteristics, Consumer Expenditure Survey, 2016-2017; Healthcare.gov. (n.d.). No health insurance? See if you owe a fee; Kaiser Family Foundation. (2017). 2017 health insurance marketplace calculator: Silver plan premiums; U.S. Department of Health and Human Services. (2015). Table VII.D.2. Average total employee contribution (in dollars) per enrolled employee for family coverage at private-sector establishments that offer health insurance by proportion of employees who are full-time or low-wage and State: United States, 2015. Agency for Healthcare Research and Quality, Center for Financing, Access and Cost Trends, 2015 Medical Expenditure Panel Survey-Insurance Component.
Sources
1
Choi, L. (2009). Financial stress and its physical effects on individuals and communities. Community Development Investment Review. Retrieved from http://www.frbsf.org/community-development/files/choi.pdf
Zurlo, K., Yoon, W., & Kim, H. (2014, May). Unsecured consumer debt and mental health outcomes in middle-aged and Oolder Americans. Journals of Gerontology, 69(3), 461–469. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24637231
Centers for Disease Control and Prevention (CDC). (2011, January 14). Health disparities and inequalities report, United States, 2011. Morbidity and Mortality Weekly Report (MMWR), 60(Supplement), 1–114. Retrieved from http://www.cdc.gov/mmwr/pdf/other/su6001.pdf
Bachrach, D., Pfister, H., Wallis, K., & Lipson, M. (2014). Addressing patients’ social needs. The Commonwealth Fund. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/fund-report/2014/may/1749_bachrach_addressing_patients_social_needs_v2.pdf
2
Bachrach, D., Pfister, H., Wallis, K., & Lipson, M. (2014). Addressing patients’ social needs. The Commonwealth Fund. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/fund-report/2014/may/1749_bachrach_addressing_patients_social_needs_v2.pdf
Robert Wood Johnson Foundation. (2011, December 1). Health care’s blind side: The overlooked connection between social needs and good health: Summary of findings from a survey of America’s physicians. Retrieved from http://www.rwjf.org/files/research/RWJFPhysiciansSurveyExecutiveSummary.pdf
3
Braverman, P., Dekker, M., Egerter, S., Sadegh-Nobari, T., & Pollack, C. (2011, May 1). How does housing affect health? Robert Wood Johnson Foundation. Retrieved from https://www.rwjf.org/en/library/research/2011/05/housing-and-health.html
University of Wisconsin Population Health Institute. (2019). County health rankings: Our methods. Retrieved from http://www.countyhealthrankings.org/explore-health-rankings/our-methods
An, J., Braveman, P., Dekker, M., Egerter, S., & Grossman-Kahn, R. (2011). Work, workplaces and health. Robert Wood Johnson Foundation. Retrieved from https://www.rwjf.org/en/library/research/2011/05/work-and-health-.html
Lynch, J., Smith, G.D., Harper, S., & Hillemeier, M. (2004). Is income inequality a determinant of population health? Part 2. U.S. National and regional trends in income inequality and age- and cause-specific mortality. Milbank Quarterly, 82(2), 355–400. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/15225332
U.S. Department of Housing and Urban Development (HUD). (2016). Breaking down barriers: Housing, neighborhoods, and schools of opportunity. Retrieved from https://www.huduser.gov/portal/sites/default/files/pdf/insight-4.pdf
Bell, J., Mora, G., Hagan, E., Rubin, V., & Karpyn, A. (2013). Access to healthy hood and why it matters: A review of the research. The Food Trust. Retrieved from http://thefoodtrust.org/uploads/media_items/access-to-healthy-food.original.pdf
4
Dube, S. R., Felitti, V. J., Dong, M., Giles, W. H., & Anda, R. F. (2003). The impact of adverse childhood experiences on health problems: Evidence from four birth cohorts dating back to 1900. Preventive Medicine, 37, 268–277. Retrieved from http://www.traumacenter.org/initiatives/Felitti,%202003,%20The%20impact%20of%20adverse%20childhood%20experiences.pdf
Mersky, J., Topitzes, J., & Reynolds, A. (2013, November). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the U.S. Child Abuse & Neglect, 37(11), 917–925. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4090696/
5
Kaiser Family Foundation. (2018, December 7). Key facts about the uninsured population. Retrieved from https://www.kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population/
6
Antonisse, L., Garfield, R., Rudowitz, R., & Artiga, S. (2018, March 28). The effects of Medicaid expansion under the ACA: Updated findings from a literature review. Kaiser Family Foundation. Retrieved from https://www.kff.org/medicaid/issue-brief/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-march-2018/
Alker, J. (2018, November 28). New report shows progress on children’s health coverage reversed course. Georgetown University Health Policy Institute. Retrieved from https://ccf.georgetown.edu/2018/11/28/new-report-shows-progress-on-childrens-health-coverage-reversed-course/
Kaiser Family Foundation. (2018, December 7). Key facts about the uninsured population. Retrieved from https://www.kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population/
7
Claxton, G., Sawyer, B., & Cox, C. (2019). How does cost affect care? Kaiser Family Foundation. Retrieved from https://www.healthsystemtracker.org/chart-collection/cost-affect-access-care/
National Association of Dental Plans. (2016). Who has dental benefits today? Retrieved from http://www.nadp.org/Dental_Benefits_Basics/Dental_BB_1.aspx
Centers for Disease Control and Prevention (CDC). (2011, January 14). Health disparities and inequalities report, United States, 2011. Morbidity and Mortality Weekly Report (MMWR), 60(Supplement), 1–114. Retrieved from http://www.cdc.gov/mmwr/pdf/other/su6001.pdf
DeLia, D., & Lloyd, K. (2014, July). Sources of variation in avoidable hospital use and cost across low-income communities in New Jersey. Rutgers Center for State Health Policy. Retrieved from http://www.cshp.rutgers.edu/downloads/10470.pdf
Centers for Disease Control and Prevention (CDC). (2016). Emergency department visits. Retrieved from https://www.cdc.gov/nchs/fastats/emergency-department.htm